Breast Reconstruction with Autologous Tissue: Natural Results Using Your Own Tissue
Breast reconstruction with autologous tissue is a highly effective option for many women after mastectomy, as it uses tissue from their own body—from areas such as the abdomen, back, buttocks, or thighs—to recreate the breast with a natural texture, shape, and feel.
Unlike restoration with silicone implants, autologous restoration offers more natural aesthetic result and long-term stability. However, this is a more complex operation, with longer recovery time and potential complications, particularly in the donor area.
When Is Autologous Reconstruction Indicated?
This method is recommended for women who:
- Desire a natural result without implants
- Have sufficient tissue available in donor areas
- Cannot or do not wish to have implants
- Have undergone radiotherapy
Not recommended for smokers, diabetics or women with vascular diseases, as there is an increased risk of complications, such as flap necrosis due to insufficient blood perfusion.
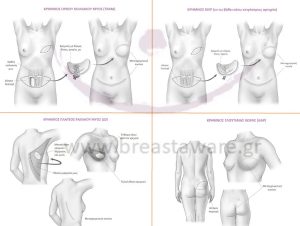
Types of Autologous Breast Reconstruction
TRAM Flap (Transverse Rectus Abdominis Muscle)
Uses muscle (rectus abdominis), fat, and skin from the lower abdomen. Provides satisfactory volume but may cause muscle weakness or hernia. Not advised for very thin women.
DIEP Flap (Deep Inferior Epigastric Perforator)
An advanced variation of the TRAM flap using only skin, fat, and blood vessels without the muscle. Requires microsurgery, but results in fewer complications and a more natural outcome.
LD Flap (Latissimus Dorsi)
Tissue is taken from the back (latissimus dorsi muscle). Often combined with an implant. Possible postoperative weakness in the shoulder or upper limb.
GAP Flap (Gluteal Artery Perforator)
Tissue from the buttocks. Used when abdominal or back tissue is unavailable. Less common and requires specialized expertise.
TUG Flap (Transverse Upper Gracilis)
Tissue from the inner thigh (gracilis muscle). Suitable for slim women, performed in specialized centers.
Autologous Fat Transfer (Lipofilling)
This technique involves harvesting fat via liposuction from areas such as the abdomen, buttocks, or thighs and injecting it into the breast. Ideal for:
- Improving small deficits after rehabilitation or radiotherapy
- Gradual volume increase with a natural effect
It usually takes 4–6 sessions, spaced 6 months apart, as a large volume of fat cannot be transferred in each session. Some of the fat is absorbed or dies. Early studies show encouraging results, but the method is still under investigation in terms of safety. long-term oncological safety.
What to Expect After Surgery?
- Longer surgical time and hospitalization in relation to implants
- Scars both in the breast and in the donor area
- Possible muscle weakness, especially with muscle-involving techniques
- Long-lasting, satisfactory, and stable aesthetic outcome
Conclusion
Autologous tissue reconstruction is an advanced, personalized solution that offers natural results and boosts confidence after mastectomy. The choice of technique is made by a team of breast and plastic surgeons based on anatomical features, medical history, and individual patient preferences.
At breastaware.gr You will find reliable and scientifically proven information about all modern options for breast reconstruction after cancer. Our goal is to support every woman to feel informed, safe and empowered on her journey.
Bibliography:
- National Comprehensive Cancer Network (NCCN)..
- Sbitany H. (2020). "Important Considerations in Breast Reconstruction and the Evolving Role of Prepectoral Implant-Based Reconstruction." J Surg Oncol. 2020;122(6):892–899.
- Eisenberg DP et al. (2022). "Comparison of Patient-Reported Outcomes After DIEP and Implant-Based Breast Reconstruction: A Systematic Review."
Plast Reconstr Surg. 2022;149(3):546e–555e. - Christodoulou EG et al. (2023)."Fat Grafting in Breast Reconstruction: Oncological Safety and Aesthetic Outcomes." Ann Plast Surg. 2023;91(2):123–129.
- Garvey PB et al. (2021). "Update on Autologous Breast Reconstruction: Indications and Techniques." Clin Plast Surg. 2021;48(1):31–44.
- American Society of Plastic Surgeons (ASPS). 2024 Clinical Practice Guidelines & Patient Resources.
